Orthostatic hypertension is an underappreciated medical condition that results in a sudden increase in blood pressure when transitioning to an upright position. If left unmanaged, it can lead to cardiovascular diseases, such as heart attacks and strokes, which remain among the leading causes of death worldwide.
However, one innovative solution that is gaining popularity in healthcare is remote patient monitoring (RPM). RPM enables healthcare professionals to remotely monitor patients, allowing for timely intervention and a reduction in the risk of serious health complications.
Understanding Orthostatic Hypertension
Orthostatic hypertension is a condition where the blood pressure rises abnormally upon standing, with a sustained increase in systolic blood pressure of at least 20 mmHg and/or diastolic blood pressure of at least 10 mmHg within 3 minutes of standing. This condition is the opposite of orthostatic hypotension, which involves a sudden decrease in blood pressure upon standing up.
Orthostatic Hypertension Causes
The condition may be caused by a variety of factors, including:
- Underlying medical conditions: Parkinson’s disease, multiple system atrophy, and type 2 diabetes have been linked to an exaggerated orthostatic pressor response, leading to orthostatic hypertension.
- Medications: Certain medications used to treat hypertension, heart disease, and depression can also cause orthostatic hypertension.
- Age-related changes: Orthostatic hypertension has been associated with hypertension in the elderly, where pressor reflexes overcompensate, resulting in higher peripheral vascular resistance and cardiac output.
- Unknown causes: In some cases, the cause of orthostatic hypertension may not be known.
Orthostatic hypertension can have significant consequences, including target organ damage and increased cardiovascular risk. Therefore, it is important to diagnose and treat the condition promptly. A normal orthostatic blood pressure response should involve an initial drop in blood pressure followed by a compensatory increase in blood pressure, which should stabilize within 3 minutes of standing. Any sustained increase in systolic blood pressure of at least 20 mmHg and/or diastolic blood pressure of at least 10 mmHg within 3 minutes of standing is considered as the accepted definition of orthostatic hypertension.
Orthostatic Hypertension Symptoms
Patients with Orthostatic Hypertension may experience a variety of symptoms, including dizziness, lightheadedness, and fainting, particularly when standing or sitting up quickly. These symptoms may be caused by venous pooling, which occurs when blood accumulates in the legs, leading to decreased blood flow to the heart and subsequent increases in heart rate and blood pressure. Other symptoms may include blurred vision, nausea, headaches, and fatigue, and they can vary in severity, affecting a person’s daily life.
Orthostatic hypertension may be due to increased arterial stiffness, which is common in older individuals. If left untreated, this condition can lead to more severe complications such as heart and kidney problems. Therefore, it is crucial for patients with Orthostatic Hypertension to seek medical attention promptly to avoid the risk of falls and injuries.
Epidemiology of Orthostatic Hypertension
The underlying mechanism of orthostatic hypertension involves the baroreflex system, which regulates blood pressure and heart rate. In healthy individuals, the baroreflex system is activated upon standing up, causing a transient increase in heart rate and vasoconstriction, which helps maintain blood pressure. However, in patients with orthostatic hypertension, the baroreflex system overcompensates, leading to an excessive increase in blood pressure. Orthostatic hypertension is most seen in elderly hypertensive patients and is associated with an increased risk of silent cerebrovascular disease. Studies have shown that there is a direct relationship between orthostatic blood pressure change and the risk of silent cerebrovascular disease in elderly hypertensives.
Orthostatic intolerance, a condition characterized by the inability to tolerate orthostatic stress, is commonly observed in patients with orthostatic hypertension. In addition, patients with orthostatic hypertension may also experience postural tachycardia syndrome, which involves a rapid increase in heart rate upon standing up. Several risk factors have been associated with orthostatic hypertension, including diabetes mellitus and essential hypertension. The exact pathophysiology of orthostatic hypertension is not fully understood, but it is thought to involve alterations in the autonomic nervous system, which regulates heart rate, blood pressure, and other vital functions.
In conclusion, orthostatic hypertension is a condition characterized by a sudden increase in blood pressure upon standing up and is associated with an increased risk of silent cerebrovascular disease in elderly hypertensives. The condition is commonly seen in elderly hypertensive patients and is associated with an overcompensation of the baroreflex system. Treatment typically involves lifestyle modifications and medication to regulate blood pressure and heart rate.
Orthostatic Hypertension Treatment
Orthostatic Hypertension is a challenging condition to manage, but there are several ways to reduce symptoms and improve overall quality of life. Here are five effective ways to treat Orthostatic Hypertension:
A. Lifestyle Changes
- Dietary Modifications: A healthy diet is crucial in managing Orthostatic Hypertension. Focus on a balanced diet that is low in sodium and high in fiber, fruits, and vegetables. Sodium can cause water retention, which can worsen Orthostatic Hypertension symptoms.
- Regular Exercise: Regular physical activity can help improve blood flow and reduce the severity of Orthostatic Hypertension. However, it is essential to start slowly and consult with a doctor before beginning any exercise routine.
- Weight Management: Maintaining a healthy weight can help reduce the risk of developing Orthostatic Hypertension and alleviate symptoms in those who have it.
B. Medications
- Fludrocortisone: Fludrocortisone is a medication that helps increase blood volume and blood pressure by reducing sodium and water loss. It is commonly used to treat Orthostatic Hypertension.
- Midodrine: Midodrine is a medication that helps constrict blood vessels, which can help raise blood pressure and alleviate symptoms of Orthostatic Hypertension.
C. Compression Stockings
Wearing compression stockings can alleviate symptoms of Orthostatic Hypertension by preventing blood pooling in the legs. This can improve blood circulation and reduce the risk of complications associated with this condition.
D. Increase Water Intake
Increasing fluid intake can help alleviate symptoms of Orthostatic Hypertension by boosting blood volume. This may help reduce the impact of changes in posture on blood pressure.
E. Remote Patient Monitoring
RPM can be helpful in managing Orthostatic Hypertension. With this technology, patients can monitor their blood pressure and heart rate from home, and healthcare providers can adjust treatment plans as needed. It can also help detect any changes in symptoms early, allowing for timely intervention.
How DrKumo Remote Patient Monitoring Helps in Treating Orthostatic Hypertension
DrKumo is a leading provider of RPM technology that can effectively aid in the management of Orthostatic Hypertension. With DrKumo state-of-the-art RPM, patients can easily monitor their blood pressure changes at home, providing valuable data for healthcare professionals to analyze and adjust treatment plans accordingly.
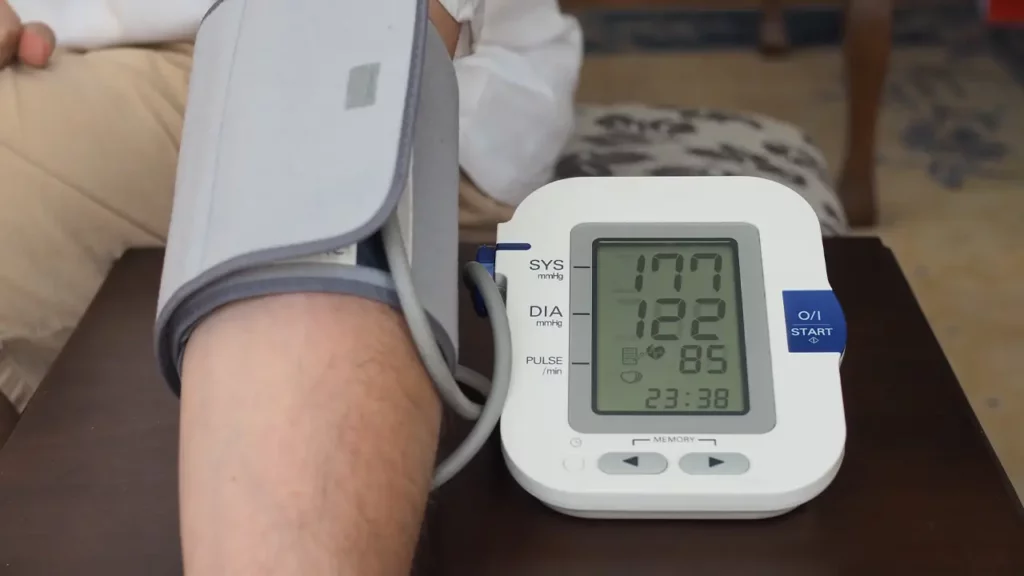
Remote Monitoring of Blood Pressure and Heart Rate
The DrKumo RPM system offers a convenient solution for elderly patients to keep track of their blood pressure and heart rate from the comfort of their homes. By utilizing a wireless blood pressure monitor and a wearable device capable of detecting heart rate and rhythm, patients can transmit their readings to their care provider in real-time. This transmission allows for easy monitoring of pressure within the cardiovascular system and any potential changes over time, enabling early identification of possible complications and timely intervention.
Alert System for Any Changes in Vitals
With DrKumo RPM solution, health professionals can receive timely alerts on any changes in a patient’s blood pressure or heart rate. This feature is particularly useful in managing Orthostatic Hypertension, as sudden spikes or drops in vital signs can indicate potential complications. By enabling healthcare professionals to receive real-time alerts, DrKumo’s solution allows for prompt and targeted intervention, preventing adverse events and improving patient outcomes. This not only enhances patient safety but also optimizes the effectiveness of treatment plans.
Moreover, the RPM solution fosters better patient engagement and adherence to treatment plans. Patients can track their vital signs and monitor their progress, enabling them to take an active role in their care. This, in turn, can improve patient satisfaction and overall health outcomes.
Takeaways
Orthostatic Hypertension can be treated through lifestyle changes, medications, compression stockings, and increased water intake. Moreover, incorporating RPM can significantly improve treatment effectiveness through remote monitoring of vitals, an alert system for changes in vitals, and better patient engagement. Seeking medical advice and timely treatment is crucial for managing the condition and experiencing improved health outcomes.
If you are interested in incorporating DrKumo RPM in your orthostatic hypertension treatment, contact DrKumo today!